News
The CDPC Final Report
The Cognitive Decline Partnership Centre (CDPC) final report “Evidence for Change: CDPC Final Report” outlines the evidence and impacts (knowledge, health, social, and economic) of the CDPC’s thirty-two research projects over the past six years.
The report highlights the research outcomes within the eight identified CDPC themes of Clinical Guidelines, Care Environment and Quality of Life, Medication Management, Attitudes to Dementia, Planning Decision Making and Risk, Maintaining Function, Sustainable Workforce, and Care Service Pathways.
CDPC submission to Royal Commission
The Cognitive Decline Partnership Centre provided a submission to the current Royal Commission on Aged Care and Quality Safety earlier this year.
Responding to the terms of reference of the Commission, the submission covers research evidence, resources and tools to deliver improved care for people with dementia.

Dementia care in the community
A new resource for use in general practice titled “People with dementia: A care guide for general practice” assists with making decisions about how to provide the best care for a person with dementia.
The guide addresses six priority topics that a GP or primary care worker is likely to encounter when providing care for a person with a dementia diagnosis.

The Consumer Voice
This article, ‘Putting the consumer in the driver’s seat: A visual journey through the Australian health‐care system as experienced by people living with dementia and their carers’, makes the case for including consumers in the design and delivery of health care.
The study conducted 25 face-to-face interviews across Australia and gathered information on how people with dementia, their family and their carers navigated their journey through the health care system.

Valuing dementia-specific quality of life states
‘How do people with dementia and family carers value dementia- specific quality of life states? This “Think Aloud” study’ is an exploration of what people and their carers value about dementia care services in relation to their quality of life.
This exploratory study is nested in a larger study that developed a new preference-based scoring algorithm for the AD-5D for people with dementia and their carers to facilitate its application in economic evaluation.

Dementia and social isolation
‘Dementia as a source of social disadvantage and exclusion’ article is based on a study that emphasises the importance of viewing dementia as not just a medical issue that we need to respond to with appropriate health and aged care but from the point of view of a social issue and explain what that social environment is like.
Given the majority of people with dementia live in the community, the article argues, that the conditions they live with and how they live is an important issue of citizenship, human and political rights. Therefore, these questions need to be examined: How do they live? How do they access services? Do their communities and friendship groups understand and accommodate them?

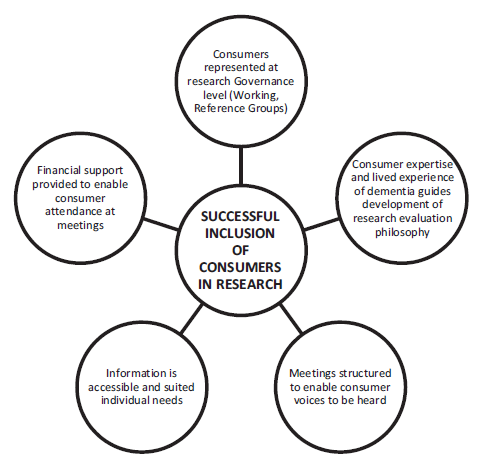
Involving Consumers in Research
‘Partnering with people with dementia and their care partners, aged care service experts, policymakers and academics: A co-design process’ examined the role of the support worker from the perspective of the person with dementia and their carer.
Consumers, industry partners and clinicians were embedded throughout the whole research process and a model of successful collaborative research was created based on consumer inclusion.
The image is a model from the article (p56) that shows the key features the research team found were key to successfully involving consumers in research.
The social impact of dementia
‘What you say and what I want: Priorities for public health campaigning and initiatives in relation to dementia,’ compared local and national campaign priorities to raise public awareness of dementia with the views of people living with dementia, family, carers and health professionals.
The study conducted in-depth interviews with representatives from local and national campaign organisations in different countries, including Australia. Interviews from the perspectives of people with dementia, carers, health and social work-related professionals and service professionals were also conducted, providing a key ‘voice perspective’.

Decision making in aged care
‘An examination of organisational policies for healthcare and lifestyle decision-making among Australian aged care providers’ examines the legislative, policy and regulatory context of residential aged care in relationship to a rights-based approach that is embodied in the Australian Law Reform Commission’s (ALRC) four Decision-Making Principles.
New aged care quality standards, applicable across all aged care settings, were introduced from July 2019, with further emphasis on rights-based approaches to decision-making that are derived from the United Nations Convention on the Rights of Persons with Disabilities (the Convention).

Aged care provider approach to regulation

Systematic review of medications in aged care
‘Process, impact and outcomes of medication review in Australian residential aged care facilities: A systematic review’ examined 13 studies of aged care facility medication reviews and argues there is a need for more data on clinical and resident outcomes of medication reviews.
Worldwide it is estimated that more than 43% of people in aged care receive potentially inappropriate medications. This is largely due to the tendency that as people age their medication regimen often gets long and complicated and can result in many medication-related problems (e.g. medication side effects or interactions between medication).

Staff structures in aged care
‘Alternative staffing structures in a clustered domestic model of residential aged care in Australia’ examines the differences in staffing structure between the traditional institutional model of aged care and the home like model of aged care, or what is referred to as the clustered model, which is consistently rated highly by consumers.
The study found that the clustered model of care had 33 per cent higher personal care attendant and hours per resident per day, 40 per cent higher staff training costs and used 14 per cent less registered nurses per day than the standard institutional model.

Hospital model responds to people with dementia
‘Implementation of a model of care for hospitalised older persons with cognitive impairment (the Confused Hospitalised Older Persons program) in six New South Wales hospitals’ examines the effectiveness of this program to improve outcomes of people with cognitive impairment when admitted to hospital.
There is a need for hospitals to have proven evidence-based procedures to manage people with delirium as more than 30% of patients aged 65 years and over present with cognitive impairment.

Volunteers reducing staff and family care burden

CDPC evaluation report
A CDPC internal evaluation report that outlines the CDPC’s performance, important learnings and evidence of implementation during the period of 2013-2018 has been released.
The Final CDPC Evaluation Report provides an in-depth examination of CDPC operations, partnerships and evidence of impact achieved over the five-year period, using qualitative and quantitative measures.

Newsletters (stories link to archived CDPC website)
CDPC Newsletter December 2019 (final)
CDPC Newsletter September 2019